Aklak
Aklak
Top of the Improvement Pops Volume 1

Welcome to our latest blog. We have searched high and low for some musical inspiration to share some desired (and less desired) improvement behaviours. Hope you enjoy our Top 20 Improvement songs, why don’t you play the track to remind you next time you encounter one these below. Enjoy!
If you have a few more tracks for your own Improvement Top 20 – let’s start Volume 2… drop us a line!
At Number 20. We don’t need another hero – Tina Turner
Tina letting us know that healthcare improvements are far better in multi-disciplinary teams. Those inspiration figures leading without coaching support can sometimes lead to unstainable improvements. And what happens when they leave?
In at 19… You’re So Vain by Carly Simon
Carly has seen a few of these. The leader/team manager who ‘knows it all’, keen to shoehorn their ‘experienced views’ whilst ‘practicing’ improvement. Often lacking a few key coaching skills
Breaking through at No 18. On My Own, By Pattie LaBelle and Michael Mcdonald
That training curriculum deadline looms. Not got time to get an improvement team together, too embarrassed to join a team so late? Nothing like doing a low-hanging fruit unstainable QI by yourself, As Pattie says ‘this wasn’t how it was supposed to be.’
In at 17. I heard it through the grape vine, by the legendary Marvin Gaye
All too common this one. Marvin in his own unique way describes the risk of relying on anecdotes and hearsay to formulate improvement aims. No proper measurements at baseline either. Oh no!
At 16, Thinking Out Loud, its Mr Ed Sheeran!
In the charts for a while now… Ed knows that it is important to brainstorm so to ‘understand the problem’ better. When not playing his guitar, he has a secret stash of sticky notes for a quick process map or fishbone to use with his improvement team.
Staying at 15, More than words, Extreme.
Don’t write pages when a few will do. Show your understanding, designs and measurements with a few choice improvement figures and run charts. Put it all together in an A3! It may engage more people than a business unit report…
A solid 14 for… Islands In The Stream, Kenny Rogers and Dolly Parton
Kenny and Dolly talk about the importance of sharing and scaling improvements properly through well designed quality management systems. Just how many isolated ward based sepsis programmes does a Trust need?
At 13, Livin’ on a Prayer, Bon Jovi.
Yep, you guessed it, random unevidenced interventions. Playing whac-a-mole until something sticks, usually under the cloud of operational pressures. Definitely ‘Livin’ on a prayer’.
Falling sharply at Number 12. Money for Nothing. Dire Straits.
Dire Straits wants you to know about starting small with your PDSAs. Don’t waste staff time and money on large scale PDSAs from the outset. Unless you want to print out 500 copies again of the wrong proforma again. There goes the budget!
Another steep drop at 11. Another one bites the dust by Queen
Freddie Mercury tells us of those Plan-Do-Study-Act cycles, where we just keep abandoning ideas because they ‘haven’t worked’. Forgetting to predict what happens in the planning phase, not taking the time to study or learn from each PDSA cycle.
Clinging on to No 10. Sitting on the dock of the bay by Otis reading
Otis is looking back on all those procrastinators and perfectionists who seem to take an eternity to move their improvements forward. Waiting for their data to come through (not SMART!), or waiting for that all important improvement team meeting in 3 months…
Up to Number 9. Shake it off by Taylor Swift.
Taylors in on it too. Just like in the Survivor track. No PDSA is a ‘bad’ PDSA. So if the PDSA doesn’t meet your prediction, learn from it and ‘shake it off’.
Straight in at number 8. Eye of the Tiger. Survivor
Put on this banging track to keep you working towards your improvement aim. Filled with resilience and perseverance, you may have some set backs, but with all that learning, you and your team will get there!
Going up to 7. Another Brick in the Wall. Pink Floyd
Pink Floyd appreciates that some improvements face many obstacles. The trick is to remove one brick at a time by breaking larger problems into smaller ones.
Falling at Number 6. The only way is up. Yazz and The Plastic Population.
We’ve all been there, those serial baseline measurements values were even lower than expected. But on the plus side, this leaves more scope to improve. Over to you Yazz!
Coming up to 5… Counting Stars by One Republic
This band knows that if you don’t measure you cannot say you have improved. They do acknowledge however that counting stars may not meet the ‘relevance’ criteria in as a healthcare SMART measurement.
Strong showing at No 4. Tow out of three ain’t bad by Meat Loaf.
Meat Loaf gets ‘very angry’ with those improvers who set challenging improvement aims from a baseline of 20% all the way to 100% in one go, in complex healthcare environments. He says set achievable expectations. Get from 20% to a new baseline of 66%, as Meat Loaf says ‘Two out of three ain’t bad’. You can always set a new improvement aim in the future.
Staying high at number 3… Levitating by Dua Lipa
Dua understands that a trend upwards of 7 consecutive measurement points in a row rarely happens by chance! The probability of that happening is 1 in 128!
Go Dua!
At number 2. I’ll Stand by you. The Pretenders,
Last week’s number one song. Through thick and thin, your improvement coach will stand by you. Fail fast, learn quick. Don’t give up. No doubt, a coach who loves their job can guide you through the whole improvement experience.
Up one place to Number 1, we have… Take a Bow by Madonna.
Madonna wants to celebrate with you! A true improvement team effort. All the stakeholders involved (including patients), a real attempt to understand the problem, clear aims and SMART measurement, using PDSA for learning. Sustaining over time, evidenced with data. All under the umbrella of continuous improvement. Take a bow!
Hope you liked this tongue-in-cheek musical podcast!
Aklak Choudhury from QIP
Join us for another blog soon!
The Twelve States of Kata

The Twelve States of Kata
As a Kata coach. I have had the opportunity to immerse myself both as a learner, a coach and sometimes a second coach. Today is not about teaching Kata, but just some personal reflections of the whole Kata process. I will be focusing on patterns of behaviours between the learner and coach which could impact on the success of Improvement Kata. In the twelve states of Kata, I have done a bit of a play on words by using ‘Kata’ each time as the first part of the word to describe the outcome or behaviour (very loosely!). I hope you will find this blog informative as a new starter to Kata and perhaps even humorous if you have been doing Kata for a while!
If you want to know more about Kata, there are plenty of resources on the web such as this one. https://www.lean.org/lexicon-terms/kata/ . I would recommend reading Mike Rother’s book on Toyota Kata too.
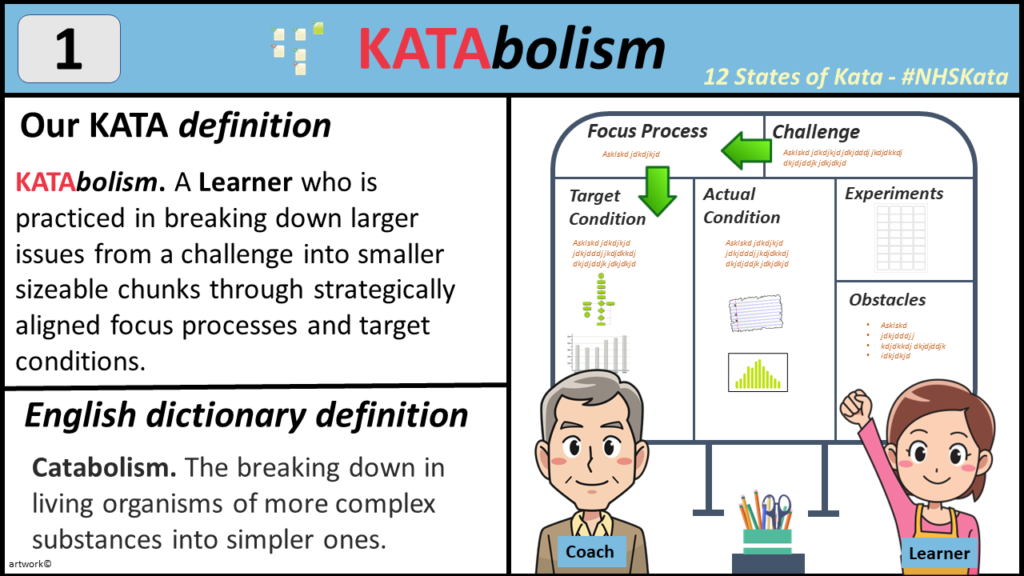
1. KATAbolism – A good thing
One of the key design features of a Kata Board is the way it enable the coach and learner to breakdown a potentially large project into smaller bite-size chunks for the learner and coach.
This is through the initial challenge statement, broken down into more specific focus processes. Then aligning each focus process into smaller target condition statements to work towards.
However, later on you will notice another dynamic with the relationships between each target condition, the obstacles that need to be over come through the experiments using PDSA cycles.
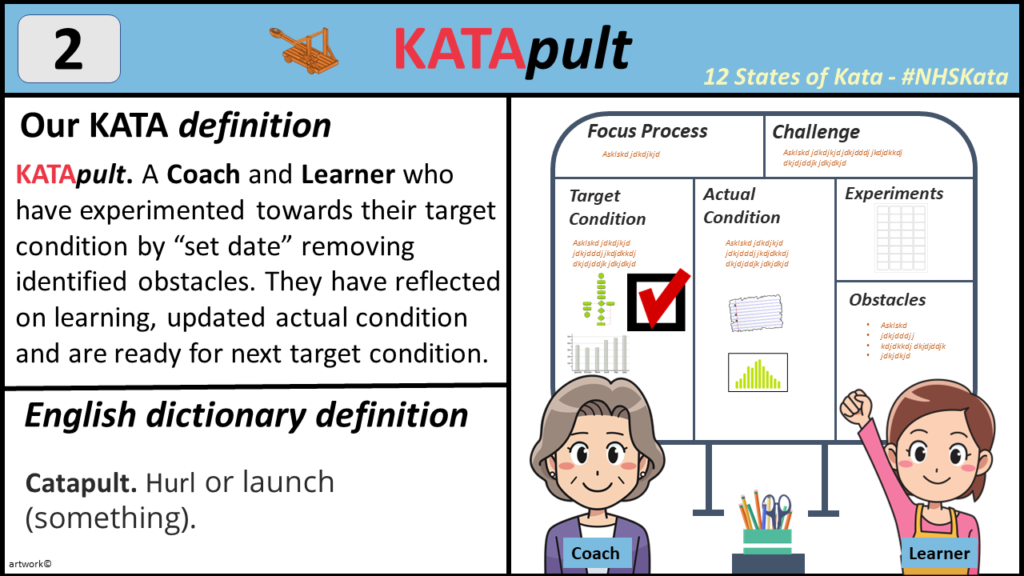
2. KATApult – A good thing
The role of the coach as to develop quickly the skills of a Kata learner. The coach enables what has been described in the Katabolism section to happen. They develop the learner’s ‘growth mindset’. Allowing learners to feel comfortable with uncertainty. Just as important is the role of the Coach to keep the learner on track. Particularly in ensuring the Target condition is SMART and in particular, achievable, within a maximum of 2-3 weeks to achieve teh target conidition.
The coach also helps ensure obstacles are related to the current target condition.
Finally, the actual condition is regularly updated to reflect the attempted improvements.
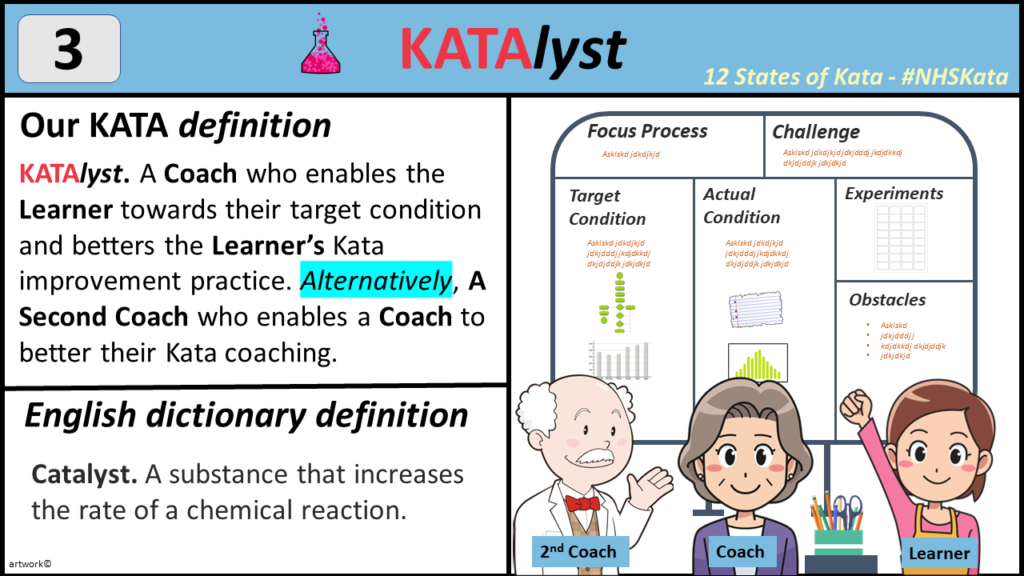
2. KATAlyst – A good thing
The coach acts as a guide to the learner, not just by systematically supporting the removal of obstacles and working towards the target condition, but also by celebrating the process in how this was achieved. The daily practice of Starter Kata with coach and learner improvement kata cycles enables a scientific approach to improvement. Similarly a well versed ‘second coach’ in Kata may pop by and observe the whole coacher-learner improvement kata cycle as a fresh set of eyes for the coach. The second coach is a formal role in developing the skills of the coach. Yes, a second Coach also a card with a set of questions to ask the coach (please remember, the learner is not present for the feedback to the coach).
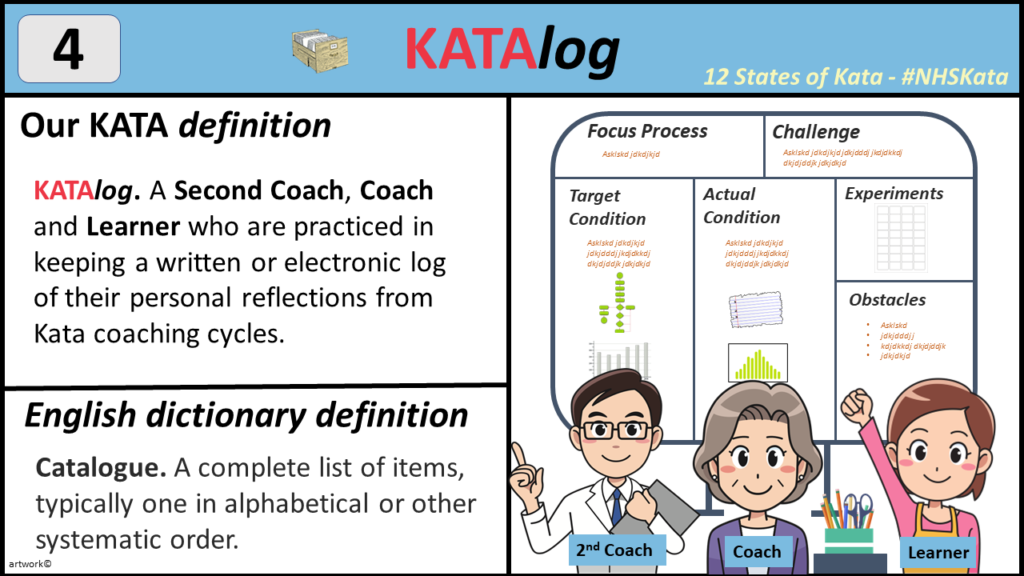
4. KATAlog– A good thing
There are some good habits that develop as a Kata learner if fully engaged in the process. One of them is to keep a record of all their personal reflections of how they felt the improvement kata cycle went with the learner. But also to record later what the reflections from the feedback from the second coach too. In my experience, it is difficult to develop the skills as a learner if you do not take time to reflect. These reflections should be written down or kept on an electronic log. These logs should be reviewed often to monitor your own development as a kata learner. The log can also sometimes be used for evidence for their Kata improvement journey.
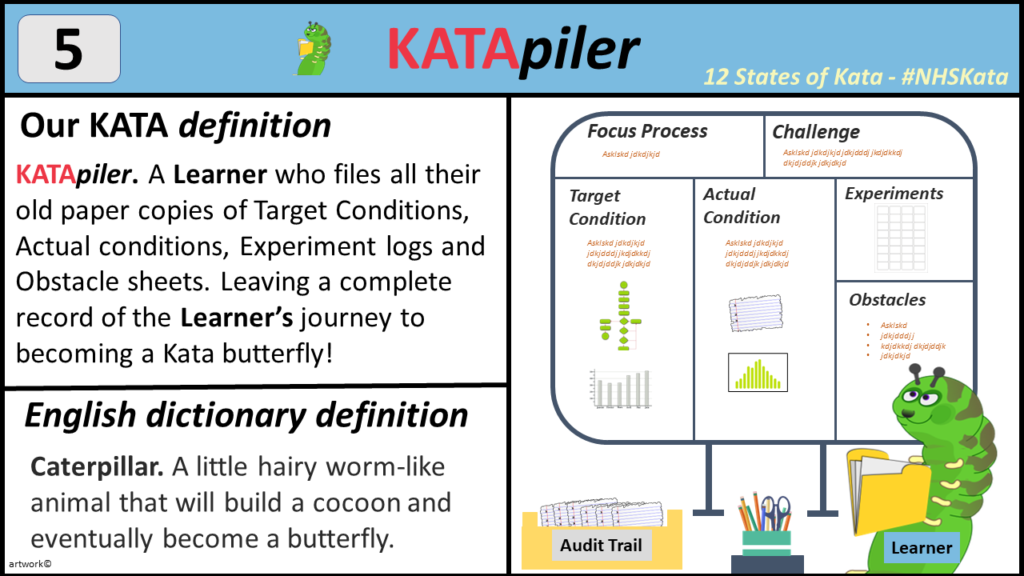
5. KATApiler– A good thing
Similar to the principles of keeping a log of your reflections. A learner should also keep a record of the old paper copies of target conditions, actual conditions, experiment PDSA logs and Obstacle sheets, Preferably in a plastic wallet or filing cabinet. They can go missing quite easily! As you develop, you can sometimes go back to them to see how you have progressed. You may find yourself saying to yourself “Wow, that target condition is so vague”, “I really didn’t update my current condition much” or “that wasn’t much of an experiment. I already knew the answer to this'”.
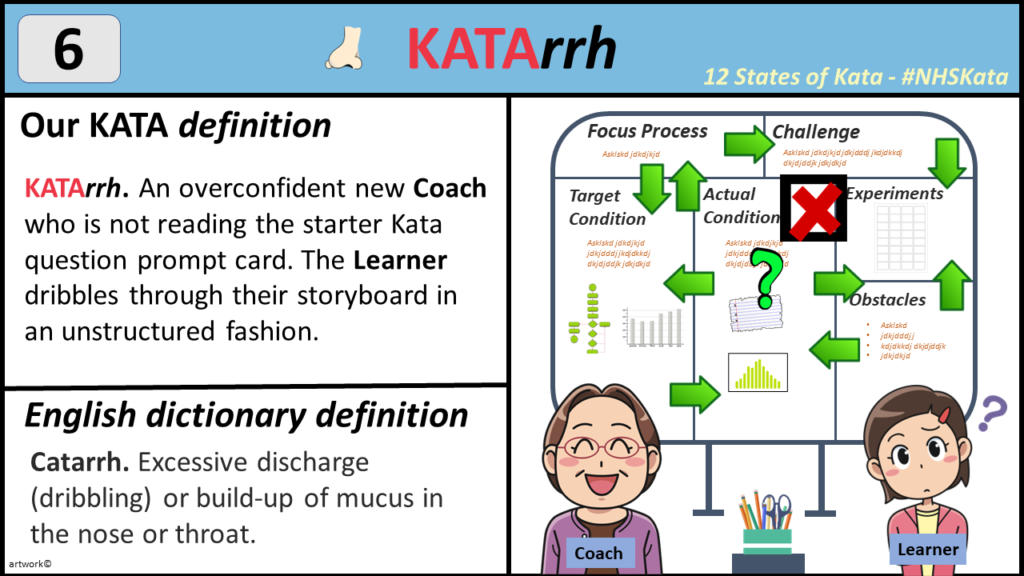
6. KATArrh– A not so good thing
Seen this a couple of times. Often from an experienced leader with the persona of “I’ve seen this all before, nothing new here”. They have an air of misplaced confidence. They are well practiced in their leadership style and it seems to work well for them. Although the coach attended all the appropriate training. They didn’t necessarily engage, take time to reflect and establish new daily practices and behaviours. i.e. the need to relearn how to ride a bike.
This is characterised by their lack of engagement with the basics, such as not reading out the Kata Card Questions in front of the learner and randomly moving around the Kata board in an unstructured fashion. This makes it very challenging for a new learner. Who has prepared diligently for the improvement Kata cycle, only to be thrown off balance.
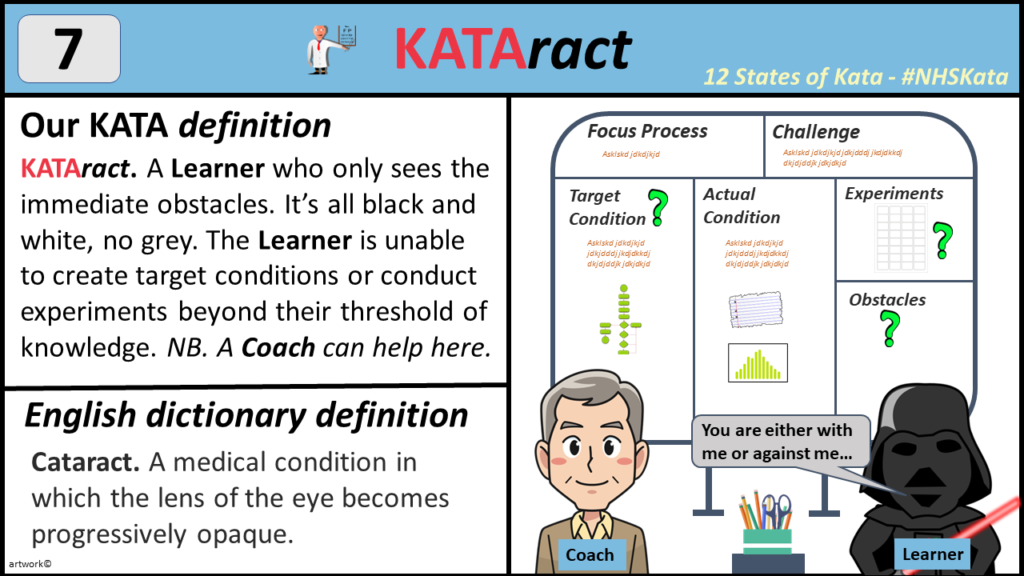
7. KATAract– A not so good thing
A learner who is attempting to engage in the Improvement Kata process. Bu they see obstacles as straightforward tasks that can be ticked off like a shopping list. These tasks are well within their scope of knowledge and experience. No need to find out more as they have the answers already.
This can be seen most observed in setting a target condition. Often stating the target condition as a solution to the problem rather than focusing on the process they are looking to improve. There is no challenge, no new learning envisaged. The learner is well within their scope of practice and residing comfortably in ‘apparent certainty‘. Rather than playing in the ‘learning zone‘. Also watch out for the ‘danger zone’ . See the diagram for Concept of a Knowledge Threshold.
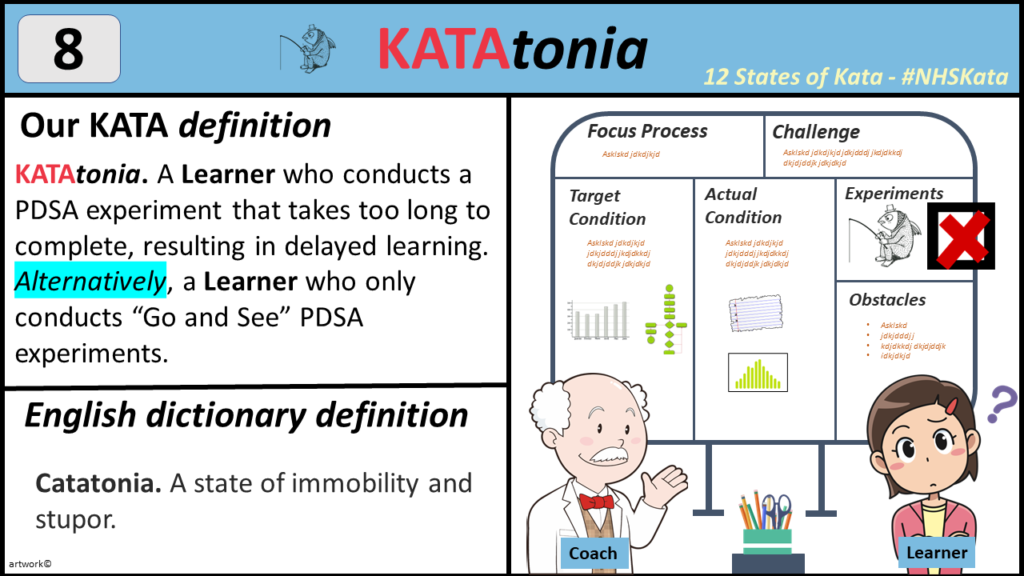
8. KATAtonia– A not so good thing
Have Learners how to conduct ‘experiments’ is a key component. These experiments are done using plan-do-study-act cycles. The experiments should be conducted to help to overcome one obstacle at a time. The learning of the PDSA cycles should be relatively quick, until the obstacle is removed. Sometime due to work shifts and annual leave. Sometimes the learner has scheduled a not so timely meeting with other staff to help resolve the obstacle. PDSA cycles can therefore stagnate.
The learner also may not be practiced in small tests of change, and end up doing a lot of ‘go and see’ observation PDSA cycles, seeking to clarify the current condition beyond reasonable doubt. The coach can help to guide the learner through this by asking the learner what small interventions can you make to know a bit more about the obstacle.
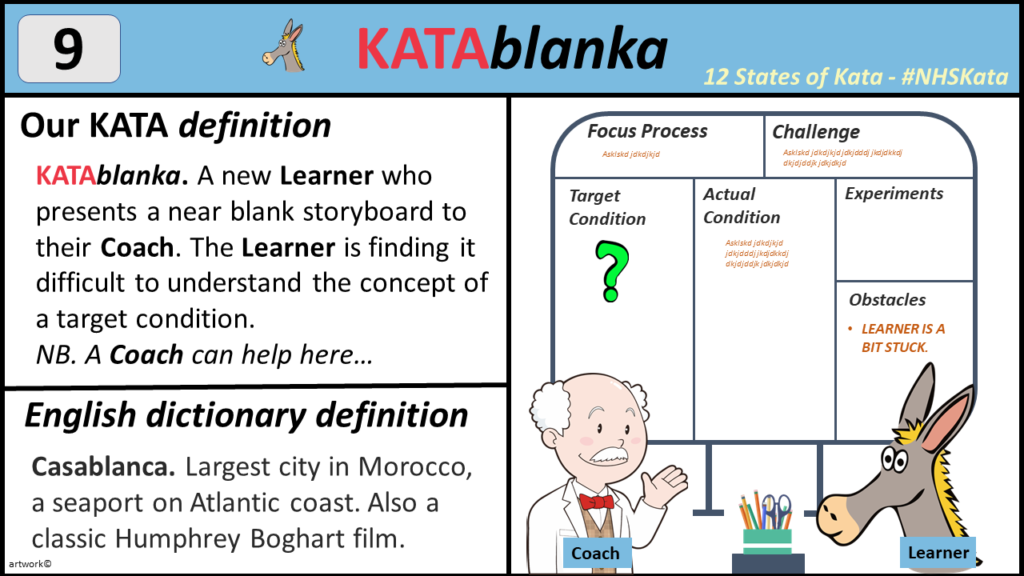
9. KATAblanka– A not so good thing
The learner has engaged with all the learning. But at the first Improvement Kata cycle, the coach encounters a near empty Kata storyboard. The learner is honest enough to say that they are finding it difficult with the concept of target condition. Here the coach will need to revisit the challenge and focus condition. This is to ensure the target conidtion aligns properly.
The coach will then focus on the elements of a target condition. This represents a desired pattern of working. Sometime represent by a high level process map. The coach will then ask the learner, what are the unique or new characteristics that will be required for this new desired way of working. And what will you measure to ensure this new process is working (outcome and process metrics).
The coach will need to make sure the Target condition is a achievable, given the timeframe of 2 to 3 weeks to complete. Has the learner bitten off too much in the Target condition?
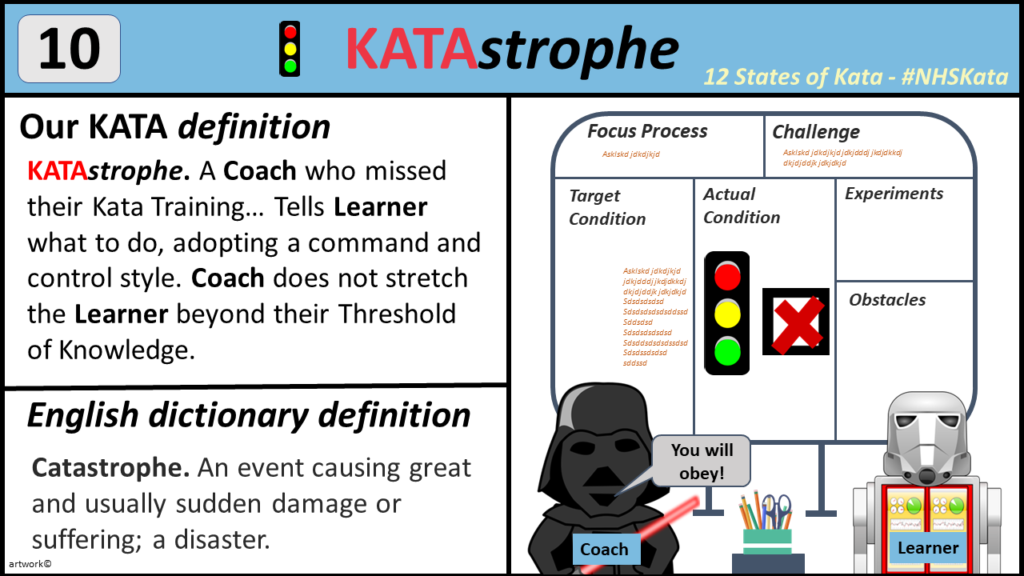
10. KATAstrophe– A not so good thing
A real disaster. A coach who has been appointed on senior their leadership role within the organisation to sponsor Kata practice. Partly to give the impression to their staff that the improvement is ‘well-led’ . Sometimes these leaders can be exceptionally busy, lots of other priorities to juggle and just did not attend or engage with the Kata training. They are used to the ‘old-school’ managerial style of hierarchical command and control. They do not allow their learners to develop, instead they say what they think the solution of an obstacle is and ask the ‘learner’ to act on it.
This is where the ‘second coach’ is a valuable resource to help reset the learning environment between coach and their learner. The coach will definitely need a lot of input. Sometimes not always succesful.
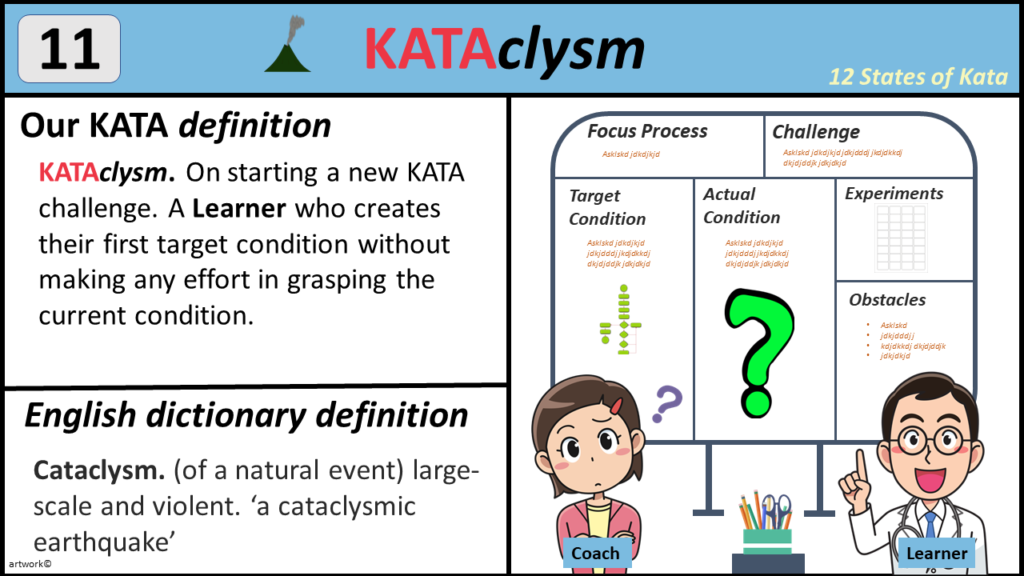
11. KATAclysm– A not so good thing
This is the learner equivalent of a KATAstrophe. In the excitement of getting going with the improvement, the learner fails to grasp the current condition. The important question of ‘where are we now?‘ has not been addressed by the learner. There is often seen by the lack of detail in the description of the ‘current condition’ section of the Kata storyboard. Was there an attempt to describe the current pattern of working with steps, sequences and time? Could you characterise the current processes. Is there measurement of process or outcome metrics?
Despite the lack of a ‘current condition’, the learner still managed to have formulated a target condition. This suggests has already formed an idea of what it is like and also what needs to change without evidence. The coach needs to guide the learner back to the beginning and describe the current decision before going further.
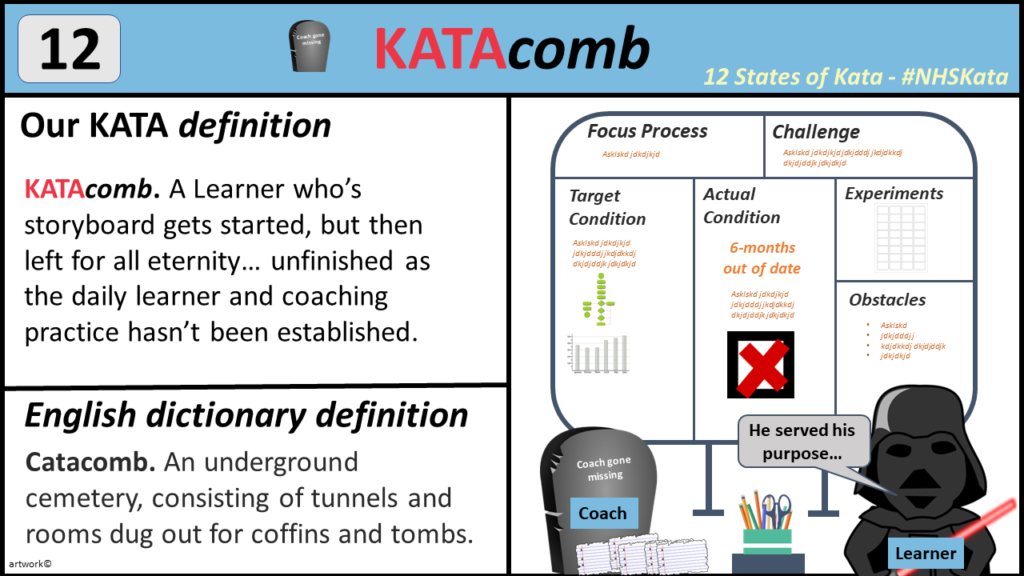
12. KATAcomb– A not so good thing
This I have seen happen a few times. The KATAcomb situation is often not related to the training of the coach or the learner. Or even their enthusiasm to practice Kata. It is often related to wider departmental and organisational drivers. If the department has not fully incorporated the improvement Kata learner coach cycles as part of their standard working of the day. It is unlikely to succeed. When a department does this well, it often replaces a previously scheduled meeting. So has the potential to be time neutral. If it feels like an artificial ‘add on’, it will not sustain.
An improvement KATA cycle with learner and coach in front of a KATA storyboard can take up to 15-20 minutes when well established (30 minutes a more for the first few cycles). One of the greatest obstacles to this is finding time, especially due to the other commitments of ‘the day job’. This is even more challenging if the coach is not the line manager of the learner, or their paths do not routinely meet as part of their working day. So this being the case, the decision of who is a learner and who should be their coach should be an active and planned decision. Almost before any training for Improvement Kata takes place. A written commitment to the learner-coach cycles and their frequency should be in place, this should be shared and agreed with more senior departmental leaders and corporate sponsors.
The final and perhaps most important driver for avoiding KATAcombs is the organisational commitment to Kata Coaching. This is almost a separate blog in itself. A lot of it is due to leadership behaviours and organisational ownership, If Kata Coaching is not part of the way we practice continuous improvement on a daily basis. It should be not just part of the improvement culture but also should have deep echoes into how we approach governance and operational challenges. A leader who inadvertently bleats out “I don’t care how you sort our the queue in Medical Assessment Unit, just get it done by tomorrow” or “we need to cancel the Kata coaching today due to front door pressures”.
I
Hope you like this weeks blog on Kata!
Aklak Choudhury
Quality Improvement Partners
Another blog coming soon by Tom Rollinson, so watch this space…
Free QI Toolkit
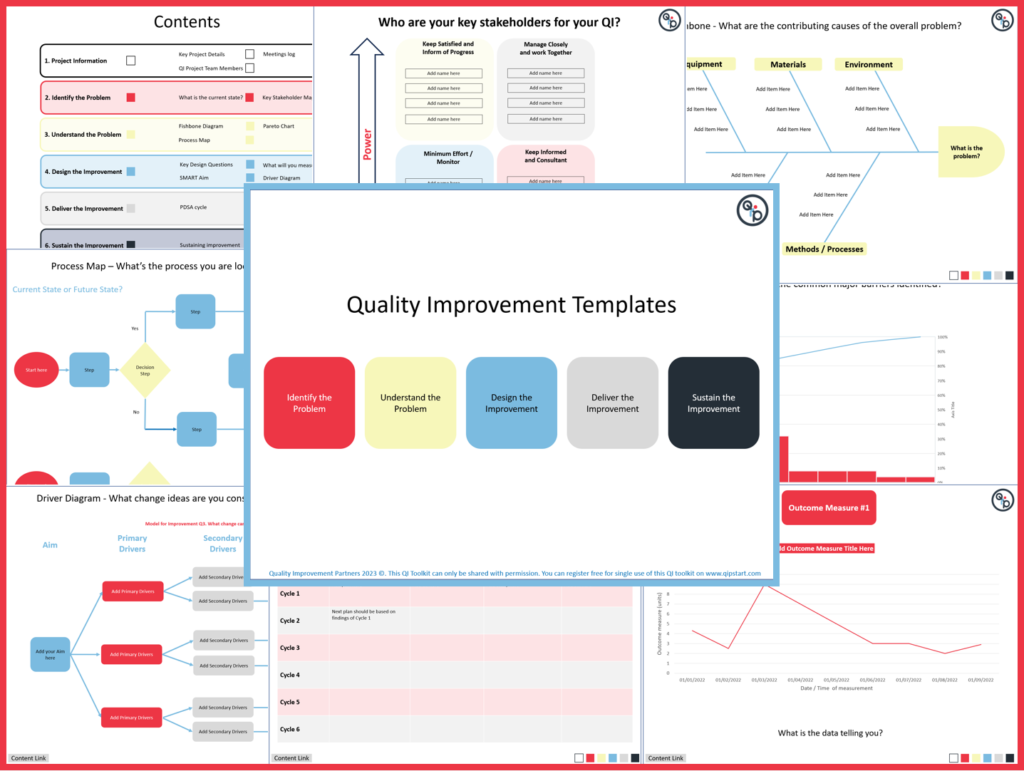
Register to get your FREE Healthcare fully editable QI Toolkit!
=
Have you every tried to keep all your resources together in one place when undertaking a quality improvement project. Especially when trying to improve the more complex problems within Healthcare. Sure there are plenty of tools out there to help. But rarely do they offer a one-stop solution to plan and deliver your improvement,
Our Quality Improvement Templates don’t just have all the most commonly used QI tools, but also…
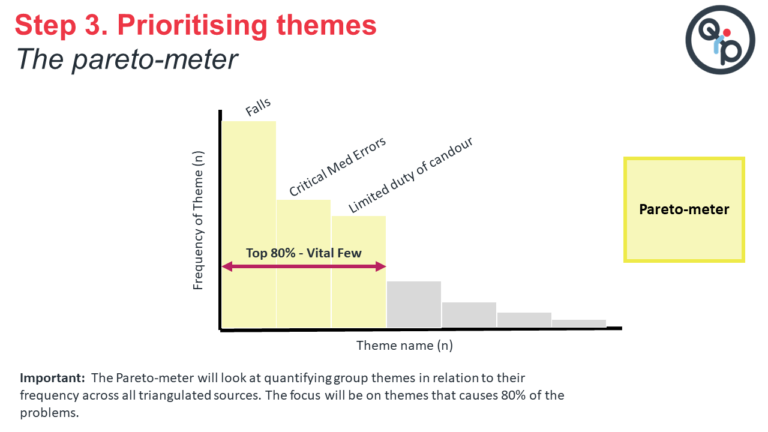
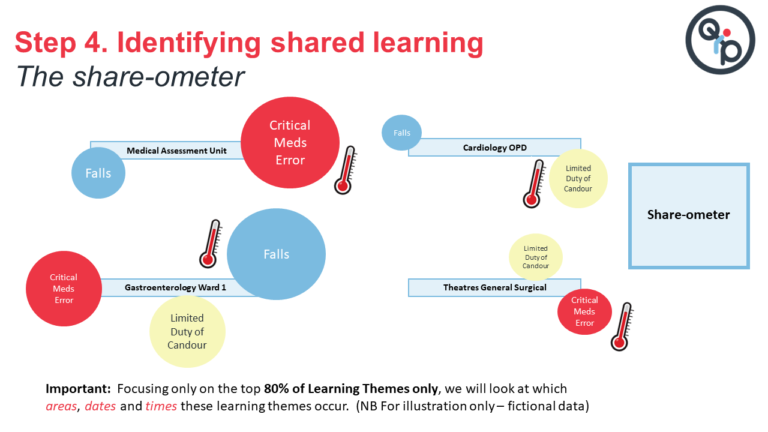
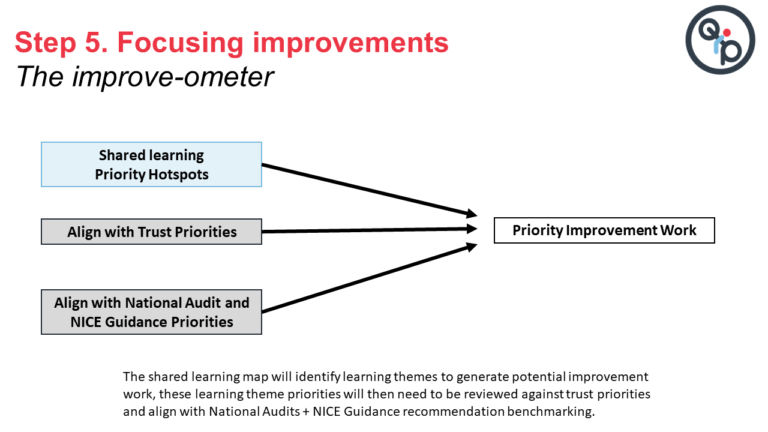
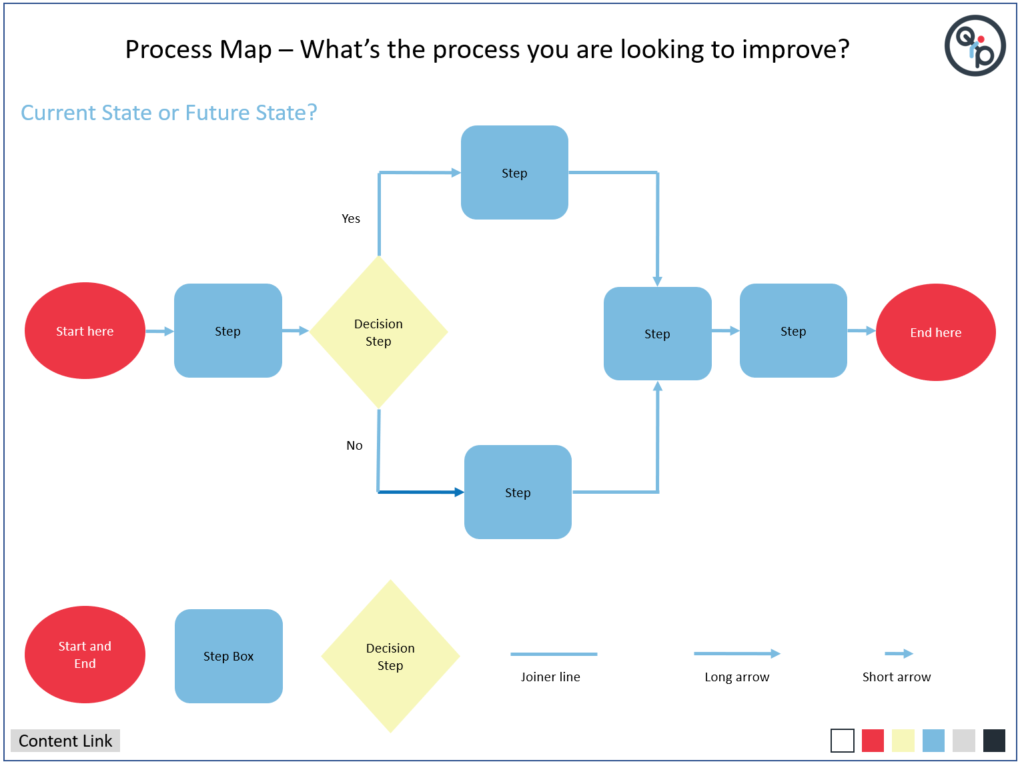
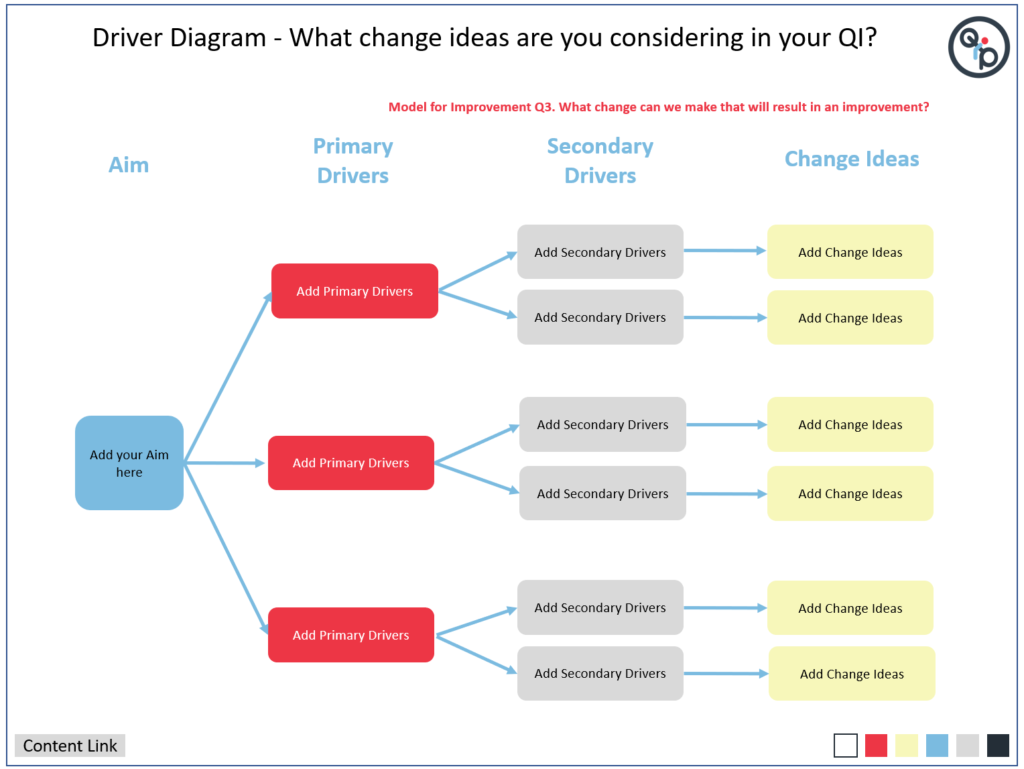
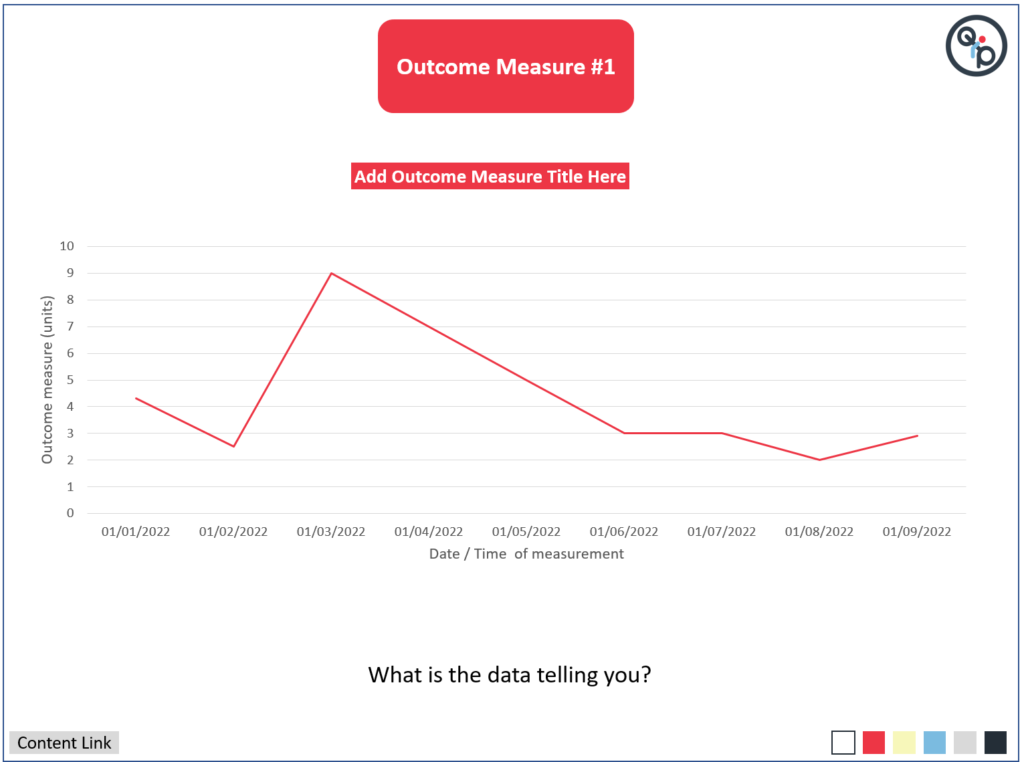
1. They are editable for you to enter information as you progress with your QI. You can create a process map, add and display data to a pareto chart or a run chart. You can describe each PDSA cycle as it happens.
2. They are shown in a logical order as to when you will encounter them. The five stages. Identify a Problem, Understand the Problem, Design the Improvement, Deliver the Improvement and Sustain the Improvement.
3. If you are a fan of Model for Improvement. The slides that indicate the 3 questions and the PDSA cycles are clearly marked in red.
4. The QI Toolkit is kept within Microsoft PowerPoint. Now how helpful is that! You can update the project at your leisure and share with colleagues either by e-mail or on a shared drive.
5. You can move rapidly across the toolkit to the correct section using the colour coded navigation boxes to update information.
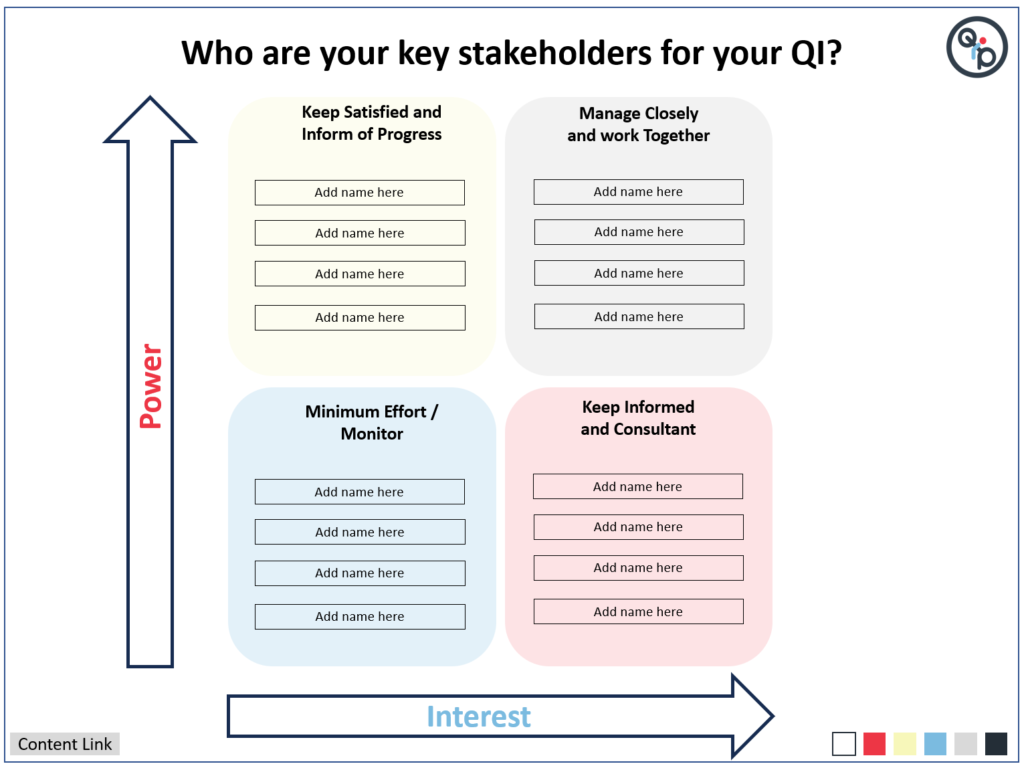
6. The QI Toolkit allows gives prompts and asks many some important questions as you progress with your QI. Such as; what is it like now? who are your key stakeholders? and what are the likely obstacles you may face?
7. The toolkit allows flexibility in what sections you will need to complete. You don’t have to use it all!
8. All the QI toolkit items, including when and how to use them are explained in our Introduction to Healthcare Quality Improvement Course.
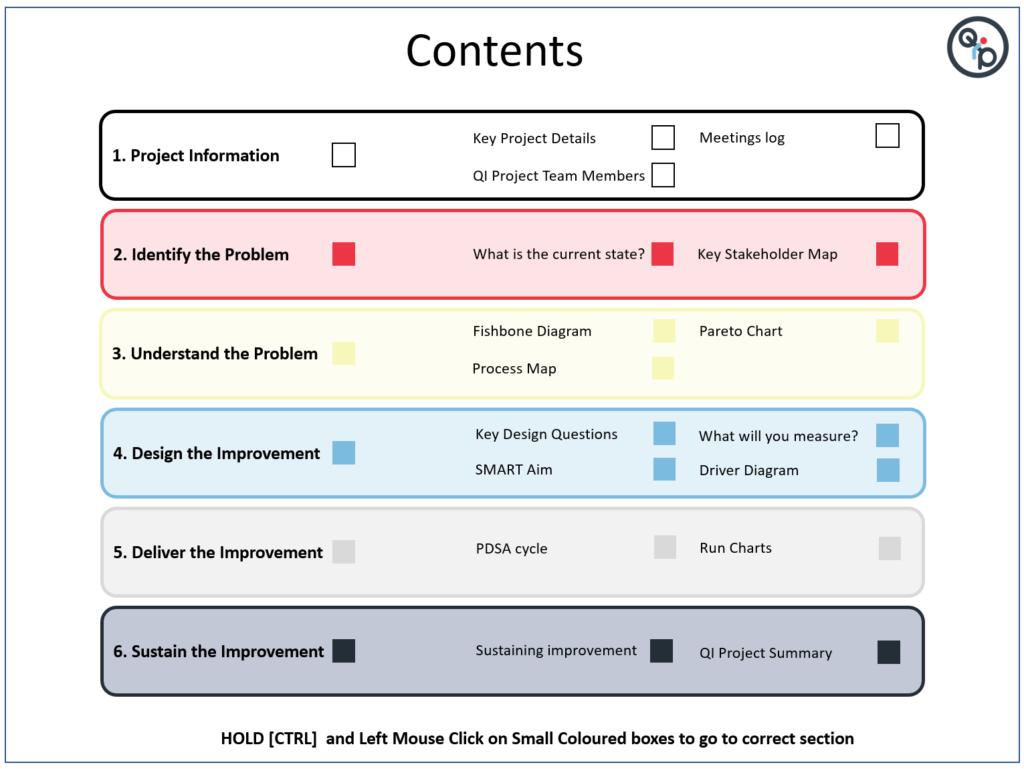
In the Deliver the Improvement Section
You will be given the tools to record your PDSA cycles and capture the measurements using run charts for outcome, process and balancing measures. Just duplicate the pages to add more run charts!
To change the data on the graph, it is just a simple case of [RIGHT CLICK] and scroll to ‘Edit Data’.
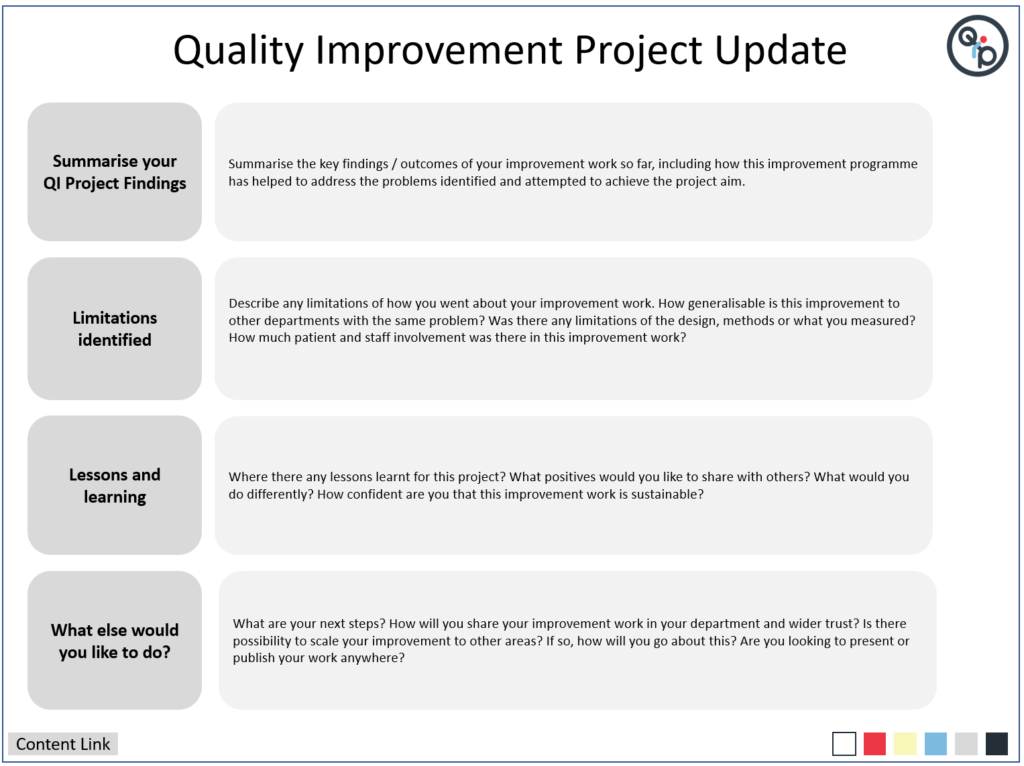
In the Sustain the Improvement Section
You will be asked to describe how you will sustain your improvement and an opportunity to provide a QI project update. this could be used as a handover document or to share with other the progress of your work so far. Remember some projects don’t ever finish as we are continually improving. So an update is all we need, rather then say we have ‘completed’ it
I
Hope you like the QI Toolkit!
Aklak Choudhury
Quality Improvement Partners
Join us for our next blog in a weeks time with Tom Rollinson
Steve from Minecraft discovers Quality Improvement
Hi Everyone, this week we will try something different!
Quality Improvement in healthcare can sometimes feel a bit disconnected to our daily working lives. It can be described in a bland unengaging way, with little opportunity to immerse yourself. Computer games have been with us for years. So why don’t we give Steve from Minecraft a go at improvement. Perhaps we can reach a wider and perhaps younger audience and make everyone curious to find out more?
In the subsequent videos you will see Steve have a go at Model for Improvement and PDSA.
Today is all about discovery…
Hope you enjoy the video podcast!
Aklak Choudhury
Quality Improvement Partners
Join us for our next blog in a weeks time with Tom Rollinson
Getting to grips with hospital QI – avoid the pitfalls!
In this week’s blog, I would like to share two podcasts describing how as a member of clinical staff you might get started with QI. I was interviewed by Rachel Saville from medical education podcast site MemCast. She also is a Respiratory Trainee Registrar in East Midlands area. Thanks Rachel! I hope you find them enjoyable. There are plenty of tips and insights for new clinicians who are beginning their QI journey. The content and links to the podcasts are described below.
Podcast 1 – Getting started with QI
Defining what the term ‘Quality’ means in healthcare through STEEEP
A definition of QI I like – ‘it’s not all about the methods’
Identifying how you should identify your stakeholders
In the world of healthcare QI, what is a mentor, sponsor and trainee
Podomatic
https://www.podomatic.com/podcasts/medeastmids/episodes/2023-07-21T05_05_47-07_00
Apple Podcasts
https://podcasts.apple.com/au/podcast/getting-started-with-qi/id1485320523?i=1000621883409
Podcast 2 – QI Steps and PDSA
Describing the five stages of an improvement programme – IUDDS
Touching base with Model for Improvement
The essence of PDSA and the common pitfalls
Some useful resources if want to know more…
Podomatic
https://www.podomatic.com/podcasts/medeastmids/episodes/2023-08-11T01_53_58-07_00
Apple Podcasts
https://podcasts.apple.com/au/podcast/qi-steps-and-pdsa/id1485320523?i=1000624135411
Hope you enjoy the podcasts!
Aklak Choudhury
Quality Improvement Partners
Join us for the next blog ‘Page Appeal, the lost art of the summary’ by Tom Rollinson next week.
Are you seriously expecting me to change the world in four months?
An experience of an F2 doctor trying to do QI in 4 months…
This might seem a bit familiar when you are starting out as the new doc on the block in a busy hospital department. You are daunted by the prospect of learning the clinical ropes. You know you need to get on with a quality improvement project, because your curriculum says so. But… you hardly know anyone or how things work around here.
Your consultant supervisor smiles innocently and asks what QI project you would like to do. You smile back and say something remotely intelligent, knowing you just lifted this off the departmental induction pack 5 minutes ago. Really you were hoping that the consultant would come out with the improvement project ideas. Surely they would be more aware of what the problems are in their department, right? But no, it is down to you.
So off you go, wondering what improvement work is out there. Asking random people, hoping someone will help you on your quest to do improvement work. That one-hour QI intro lecture at the beginning of the year seems a distant memory.
In the first month, most of your time is spent trying to keep your head above water. You often feel overwhelmed. There is just so much to know and learn. Trying to start a QI project seems less of a priority when compared to the clinical work pressure. You want to be safe for your patients… You will think about QI later. A form of ‘duality’ occurs in your mind. The need to separate the clinical work to that of the improvement work. Yes, to compartmentalise will help you cope and get through the day. You will leave the ‘QI bit’ to Thursday afternoon when the staffing is better and it is quieter.
You become more aware that you are a now a small cog in a team you are not familiar with. Some staff have been there for years, some have just started, just like you. A few weeks pass, you are getting to know all the players; who is important in the team, who can help and who to avoid. But as a relatively new doctor, you don’t feel safe proposing any improvement ideas to the team. How will they react to your idea? Will you end up looking foolish amongst your peers? Can you speak up to your consultant surgeon with many years experience and say there might be a problem worth fixing? Do they even care what you think? Do you feel psychologically safe enough to bring this up??
The 4-month rotation mercilessly moves on. A few on-call weekends pass. It is already week six. Not much has happened on the QI front. Some ideas form, but nothing concrete. So much for the flying start… a few more weeks pass. You begin to feel more comfortable within the department, you know your role within the team. Importantly, you are now developing relationships with your ward nurses, physios and pharmacists. One or two are now your friends.
A few more weeks pass. The clinical work pressures remain, but you are performing well clinically, you have formed an identity and feel valued for your work. You begin to revisit your need to complete a QI project. This is your last rotation for the year, your ARCP assessment is just around the corner. You wanted to make a meaningful impact on patient care through QI, but now there is not enough time. Perhaps you should focus on something that is more manageable? Try to keep the improvement small, the change ideas simple. Maybe focus on some ‘low-hanging fruit’ QI. Possibly a stool chart PDSA, or perhaps a handover sheet for the morning surgical meeting. You could print the sheets out yourself. No need to get the wider team involved. The QI might not sustain after you leave, but at least it is something you can show at ARCP. You will try and do a ‘proper’ QI next year.
The 4-month rotation is now up. The QI project done. A couple of PDSA cycles mashed together. The time-sensitive ticking clock of QI negated, just in time for ARCP. But the QI ticking clock has now been replaced by another type of ‘tick’. The all too familiar QI tick box
The above story is fictional. It is based on the findings of a qualitative MSc study exploring how the social learning environment influence how trainee doctors engage with improvement work (Choudhury 2022). F2 doctors, educational supervisors and trust improvement specialists were interviewed.
We can explore the challenges that F2 doctors face immersing themselves within a new clinical department through the lens of Tuckman’s team building model (Tuckman 1965). The model described a number of stages for team development.
Forming – a new team is formed with rotational doctors joining every 4 months. Tasks and roles are not always defined.
Storming – Individual boundaries become contested and conflicts can occur. There is often jostling for position for new staff.
Norming – Members of the team resolve their differences, with greater acknowledgement of other team members strengths and weaknesses
Performing – The team becomes functional, works effectively and efficiently to complete tasks. There is high development of roles and responsibilities
Adjourning – This phase does not always occur. Especially for junior doctors, as they are often not there long enough. Can lead to missed opportunities to celebrate successes or even mourn their departure.
The illustration below highlights the strain for F2 doctors when faced with the competing priorities of performing clinical duties and improvement work all at once during a four-month placement.

So what does this all mean?
These F2 doctors describe an uncomfortable feeling of a clock ticking down with growing pressure to complete a piece of improvement work within a four month window. This is challenging for an established member of a departmental team, but near impossible for new members such as F2 doctors.
So why the mad rush to finish the QI project in 4 months? We know that complex problems can often take many years to improve often under the umbrella of continuous improvement. A more systematic sustainable approach to improving quality of care, with no obvious start or end date to the improvement programme.
Could there be extrinsic drivers to explain this behaviour? F2 doctors can describe in detail the scoring systems for QI and clinical audit with their relative weighting for shortlisting. Just as an example, the specialist interview shortlisting for physician higher training for QI attainment suggests to score the top prize of 5 shortlisting points, you need cover:
“all aspects of two [PDSA] cycles where you can demonstrate a leadership capacity by supervising other members of the team.”
Wow… that would be an impressive feat considering it takes three months to get your feet under the door in a new department! Did I mention, the F2 doctor will also need to lead and inspire these departmental old-timers in a QI programme… I hope they had all their leadership experience front-loaded in medical school.
Training curricula for doctors can also be overly prescriptive in what constitutes ‘exemplary standard’ of QIP. Let us take the example from physician core training assessment tool for QI.
“QIP topic related to an important clinical problem, detailed and exhaustive methodology applied, appropriate presentation of results with correct interpretation and comprehensive conclusions. Plans for future direction of QIP highlighted. An exemplary QIP.”
All of the above in 6-months for internal medical trainees, a lot to do and not a mention of a team approach to QI anywhere…
So have we set-up our new doctors to fail? To achieve the unachievable? Have they signed up to Mission Improbable? The educational and competitive career progression mandate has led to trainees seeing QI as a hurdle to overcome and not seeing improvement for what it should be, an opportunity to improve the patient experience. It is in fact us who have led them to the ‘QI tick box’. That short term unsustainable ‘low hanging fruit’ piece of QI work done in haste, that has little impact on patient outcomes.
So what could we do differently?
Certainly there is recognition for change. It was encouraging to see the recent publication from the Academy of Medical Royal Colleges and their take on assessment of QI published in 2023. The document states trainees are not required to have done entire projects from start to finish (phew!), and there was no need to lead a project at any stage of training (double phew!).
This change in direction can be a catalyst for major quality improvement reform for doctors in training. It is badly needed. NHS organisations need our rotational trainee doctors to support the often complex challenges facing many trusts. They are the ones seeing the problems daily, why should they not be part of the response?
We can help our trainee doctors by:
Promoting at trainee induction the correct mindset for improvement, specifically, that meaningful QI participation in results in better patient experience
Identify departmental improvement work early in their four-month rotation. They should not be searching for it
Allow trainees to remain on improvement programmes for greater than four months when feasible, if not possible, ensure mechanisms for handover of their QI work
Create multi-disciplinary coaching and support groups for rapid onboarding of new doctors through a departmental QI Faculty
NHS trust corporate teams could ensure local departmental improvement work is recognised and appropriately supported rather, rather than focus solely on executive driven large scale programmes