As the field of Quality Improvement grows year on year, new and interesting methods are developed as a way to support improved quality for patients care. Many of these emanate from different industries and have been adapted for health care. The ever growing list of methods can seem confusing when first getting started and creates tension over whether you are using the right one. To help with this, we have outlined a list of methods which are more commonly used, a short explanation and where you can find out more information:
QI Method
What is it?
Breakthrough Collaboratives

Breakthrough Collaboratives, led by the Institute for Healthcare Improvement (IHI), are focused, time-limited initiatives that bring together healthcare organisations to achieve rapid and substantial improvements in specific and pre-determined areas of healthcare quality and safety. Participating organizations collaborate, learn from one another, and implement changes to address common challenges. They use data, structured learning, and peer networking to accelerate improvements. The aim is to achieve significant, large-scale changes that benefit patient care and safety with a focus on spreading successful strategies to other organizations and sustaining improvements over time.
Learn More: https://www.ihi.org/resources/Pages/IHIWhitePapers/TheBreakthroughSeriesIHIsCollaborativeModelforAchievingBreakthroughImprovement.aspx
Clinical Audit

Clinical audit helps to align care and benchmark against known standards, enhance patient safety, and ensure efficient and effective healthcare delivery. Clinical audit involves evaluating clinical practices, identifying areas for improvement, implementing changes, and monitoring progress. Key steps include defining objectives, collecting and analysing data, identifying discrepancies, making recommendations, implementing changes, and continuously reviewing and learning from the process.
Learn more: https://www.hqip.org.uk/wp-content/uploads/2018/02/developing-clinical-audit-patient-panels.pdf
Experience based co-design
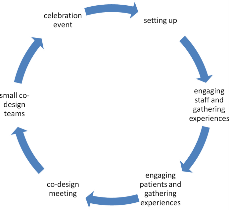
Experience-based co-design (EBCD) is a collaborative approach used in healthcare service design, involving patients, staff, and families. It identifies issues in healthcare delivery, hosts co-design workshops to brainstorm solutions and iteratively tests and refines these solutions. EBCD emphasizes a patient-centred culture. It transforms healthcare by integrating patient and staff feedback to enhance care quality and satisfaction.
Learn more: https://www.pointofcarefoundation.org.uk/resource/experience-based-co-design-ebcd-toolkit/step-by-step-guide/1-experience-based-co-design/
Lean
Lean is a management philosophy and methodology that originated from manufacturing and has since been applied to various industries, including healthcare. It focuses on eliminating waste, improving efficiency and maximising value for customers or patients. Key principles of lean include identifying and reducing non-value-added activities, continuous improvement, empowering employees to contribute to problem-solving and creating a culture of efficiency and quality. Lean techniques, such as value stream analysis, 5S (Sort, Set in order, Shine, Standardize, Sustain), and Just-in-Time production are used to streamline processes and enhance productivity. Lean aims to deliver higher quality outcomes while reducing costs and resource waste.
Learn More: https://www.lean.org/explore-lean/what-is-lean/
Learning from Excellence

‘Learning from Excellence’ is a healthcare quality improvement approach that focuses on studying and extracting lessons from instances of excellence and exceptional care within the healthcare system. Unlike traditional quality improvement methods that primarily emphasize analysing errors and adverse events (often referred to as “safety I”), “Learning from Excellence” shifts the focus to understanding and replicating what goes right in healthcare delivery (often referred to as “safety II”).
Learn More: https://learningfromexcellence.com/about/
Learning from Incidents

‘Learning from incidents’ begins with prompt incident reporting and thorough analysis to identify root causes and contributing factors. From this analysis, actionable recommendations for improvement are formulated and implemented, including adjustments to protocols, training enhancements, or equipment upgrades. Continuous monitoring ensures that changes lead to improved emergency responses, while knowledge sharing fosters a culture of improvement. Ongoing training is provided based on incident findings, and protocols are regularly reviewed and adapted to address emerging challenges, ensuring that service remains responsive and effective in delivering critical care.
Learn more: https://qualitysafety.bmj.com/content/26/3/252
Model for Improvement

The Model for Improvement is a framework used to systematically improve processes. It involves asking three key questions: What are we trying to accomplish (Aim)? How will we know a change is an improvement (Measures)? What changes can we make to achieve improvement (Interventions)? And then uses a four-step cycle in an iterative approach to work towards the aim set: Plan (identify and plan changes), Do (implement changes on a small scale), Study (analyse results), and Act (decide whether to adopt, adapt, or abandon changes).
Learn More: https://www.ihi.org/resources/Pages/HowtoImprove/default.aspx
Operational Excellence / Quality Management System (QMS)

A Quality Management System (QMS) is a structured framework within an organization to consistently meet or exceed patient expectations and adhere to quality standards. Quality Management systems are becoming more popular within the healthcare sector and typically consist of several key components:
Quality planning – Collectively agreeing what the overall System (or organisation) wants to deliver and how to do this
Quality Assurance – checks which are put in place to ensure quality of care is being delivered using verified evidence and articulating improvements which have bene made, or areas for further focus
Quality Control – the way monitoring and maintenance occurs to ensure that we know whether the system is achieving the outcomes required
Quality Improvement – the systematic approach used to make tangible change and improve performance
This draws heavily on Lean methodology, adapted for healthcare.
Learn More: https://kpmg.com/xx/en/home/industries/healthcare/operational-excellance-in-healthcare.html
QSIR

QSIR, which stands for “Quality, Service Improvement, and Redesign,” is a comprehensive healthcare approach aimed at improving patient care and outcomes. This is a dedciated set of training courses (depending on your experience) and repository of tools and techniques which can be used to enhance quality standards, streamline service delivery for efficiency and effectiveness, and foster innovative process redesign. Utilising tools such as process mapping and improvement cycles like Plan-Do-Study-Act (PDSA), QSIR promotes a consistent understanding of QI tools which can be used and aims to standardise QI in the NHS.
Learn More: https://aqua.nhs.uk/QSIR/
Six Sigma

Six Sigma is a data-driven approach used for process improvement and quality management across various industries. It aims to reduce process variations and defects, ensuring consistent high-quality outcomes. Six Sigma follows a structured approach known as DMAIC (Define, Measure, Analyse, Improve, and Control) and emphasizes data-driven decision-making, customer focus, and continuous improvement. Trained professionals, known as Black Belts and Green Belts, lead and support improvement projects. The ultimate goal is to enhance quality, reduce costs, and achieve customer satisfaction through empirical evidence and ongoing optimisation.
Learn more: https://www.youtube.com/watch?v=4EDYfSl-fmc&ab_channel=Simplilearn
Toyota Kata

Toyota Kata is a structured improvement and coaching routine developed by Toyota. It involves understanding the current condition, setting a target condition, experimenting, and iterating toward improvements. Leaders provide direction and challenges, while the Improvement Kata and Coaching Kata routines guide teams through the problem-solving process. The PDCA (Plan-Do-Check-Act) cycle is integral to the approach, and a fundamental principle is the respect for people, encouraging collaboration and shared responsibility for continuous improvement.
Learn More: http://www-personal.umich.edu/~mrother/Homepage.html
Virginia Mason Improvement Approach

Virginia Mason’s improvement approach, often associated with the Virginia Mason Production System (VMPS), is a healthcare approach that focuses on continuous improvement, patient safety, and delivering high-quality care. Key elements of this approach include a patient-centric culture, Lean principles, and interdisciplinary teamwork. It aims to streamline processes, eliminate waste, engage staff, and enhance patient experiences. This draws heavily on Lean methodology, adapted for healthcare.
Learn More: https://www.virginiamasoninstitute.org/resource/case-study-bringing-impact-within-reach/
This is not an exhaustive list and there are many other methods which have been used to improve patients care. but we wanted to give a general view of the ones which have been used/work in our experience. However, the next step in picking which one to use can be daunting for fear of picking the wrong one. The evidence on which QI method is most effective is ropey and although certain methods have more documented examples or publications, it is still far from consensus on which one works best. However, it is important to remember that many share underlying principles including:
Identifying the problem which is affecting quality
Analysis of the problem
Setting a clear and specific goal to work towards
Developing a theory of change
Identifying change ideas and testing these changes out in a iterative fashion
Developing interventions to sustain improvements, where needed
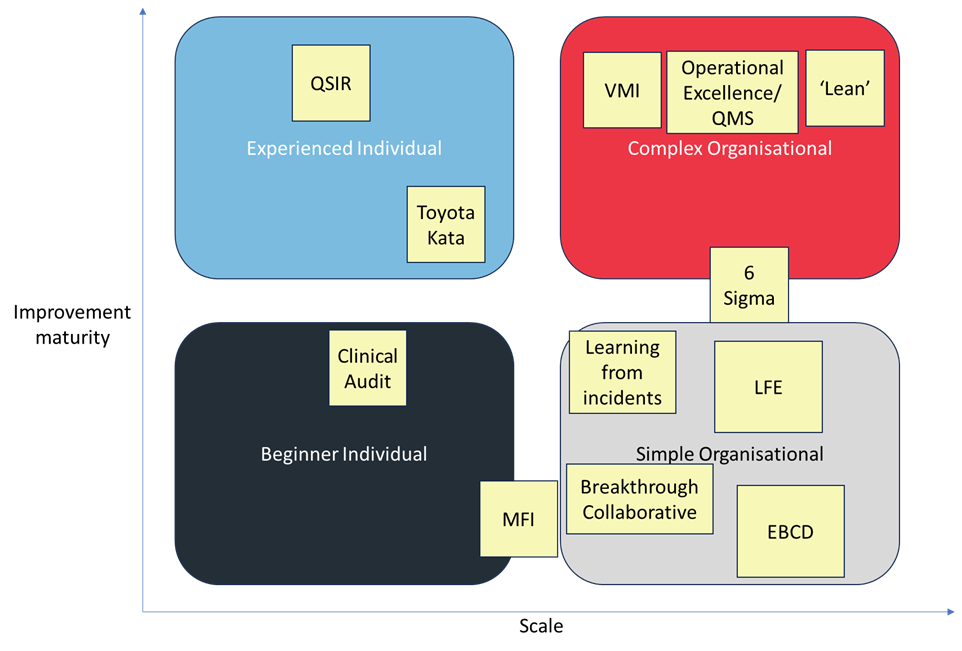
Despite similarities in principles, different approaches may be used depending on the scale of the improvement effort as well as the capability maturity with improvement methods. We have visualised this below and is our view on how this generally works. It would be great to hear if you think differently, so we can learn from you!
In our opinion, the important thing is just pick one approach and get started. Try it out, learn from using it and adapt the approach to what works for you. There will never be a one size fits all which suits your style and circumstances, so the key is take what is useful and adapt in true PDSA fashion.