This was the question posed to me, by a senior leader in an organisation when we were thinking about how we should work with some high performing areas, as opposed to just focusing on the ones more challenged…
“Learning from Excellence” (LfE) and “Safety II” are both concepts that have emerged in the fields of healthcare and safety management. While some might perceive them as “wet” or “happy clappy”, they actually represent significant shifts in mindset towards proactive approaches to learning and improvement, rather than focusing solely on why things go wrong. Here’s why they’re important and why attention should be paid to them:
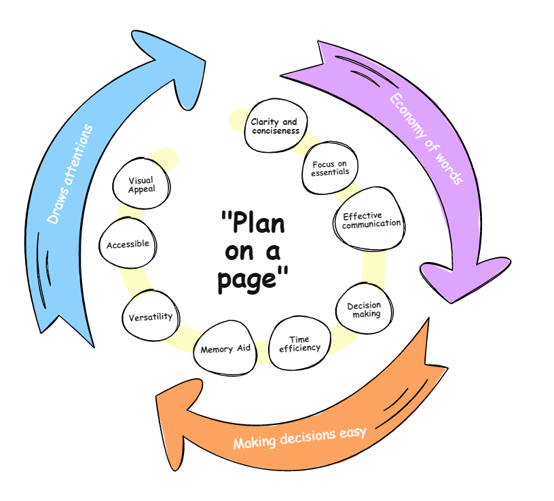
Focus on Positives: Traditional safety and quality improvement efforts often focus on identifying and mitigating errors or deficiencies. LfE, on the other hand, emphasizes learning from instances of excellence or success. Far and away, things go right more than they go wrong, which is a cause for celebration. By studying what goes right, organizations can identify patterns and practices that contribute to positive outcomes, enabling them to replicate and build upon them.
Proactive Approach: Safety II, a concept developed by Erik Hollnagel and others, emphasizes understanding how systems function under normal conditions and what contributes to their resilience. Instead of solely focusing on preventing failures, Safety II seeks to understand how systems adapt and recover from challenges. This proactive approach can help organizations anticipate and mitigate potential risks before they escalate.
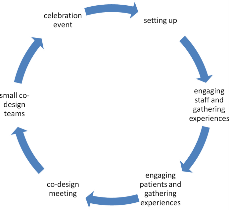
Culture of Learning: Both LfE and Safety II promote a culture of learning and improvement. By encouraging reflection, open communication and a willingness to learn from both successes and failures, organizations can create environments where continuous improvement becomes the norm. This can lead to better patient outcomes, safer work environments, and more efficient processes.
Employee Engagement: Emphasizing excellence and proactive safety measures can also increase employee engagement. Rather than the “brow beating” repetition of telling people they have done it wrong, Safety II changes the narrative to have positive discussions about what went well. When employees feel empowered to contribute ideas and participate in improvement efforts, they are more likely to take ownership of safety and quality outcomes. This can result in higher morale, lower turnover rates, and increased productivity.
Resilience: By understanding how systems function under normal conditions and what contributes to their resilience, organizations can better prepare for unexpected events or crises. This can help mitigate the impact of disruptions and improve overall organizational resilience.
With this, there are several recent high profile initiatives led by the highest levels of the NHS England, which have focused on learning from the “best in class” such as Ambulance handovers and Staff Survey across the UK. Although this is still fairly new to the NHS, this shows the departure from old ways of working to a more sustainable and empowering approach.
In summary, while Learning from Excellence and Safety II may represent a departure from traditional approaches to safety and quality improvement, they offer valuable insights and methodologies for creating safer, more resilient and more efficient organizations. Paying attention to these concepts can help drive meaningful change and improve outcomes in a variety of industries. This isn’t to say that we shouldn’t review when things go wrong, however it represents a shift in balance in the conversations about the things that went well, which account for the vast majority of occasions.
My response to said senior leader was… “I think we have some work to do”